Reading Time: 5 min.
Safety in medication therapy is fundamental in clinical hospital management. Errors in the prescription, transfer, distribution and administration of drugs can have serious consequences. To avoid such negative outcomes, it is necessary for hospitals to invest in a customized medication management system. A fully electronic-based system that records and organizes medication from admission to discharge significantly reduces medication errors. Closed loop medication management (CLMM) with unit dose dispensing is the optimal approach.
What is closed loop medication management?
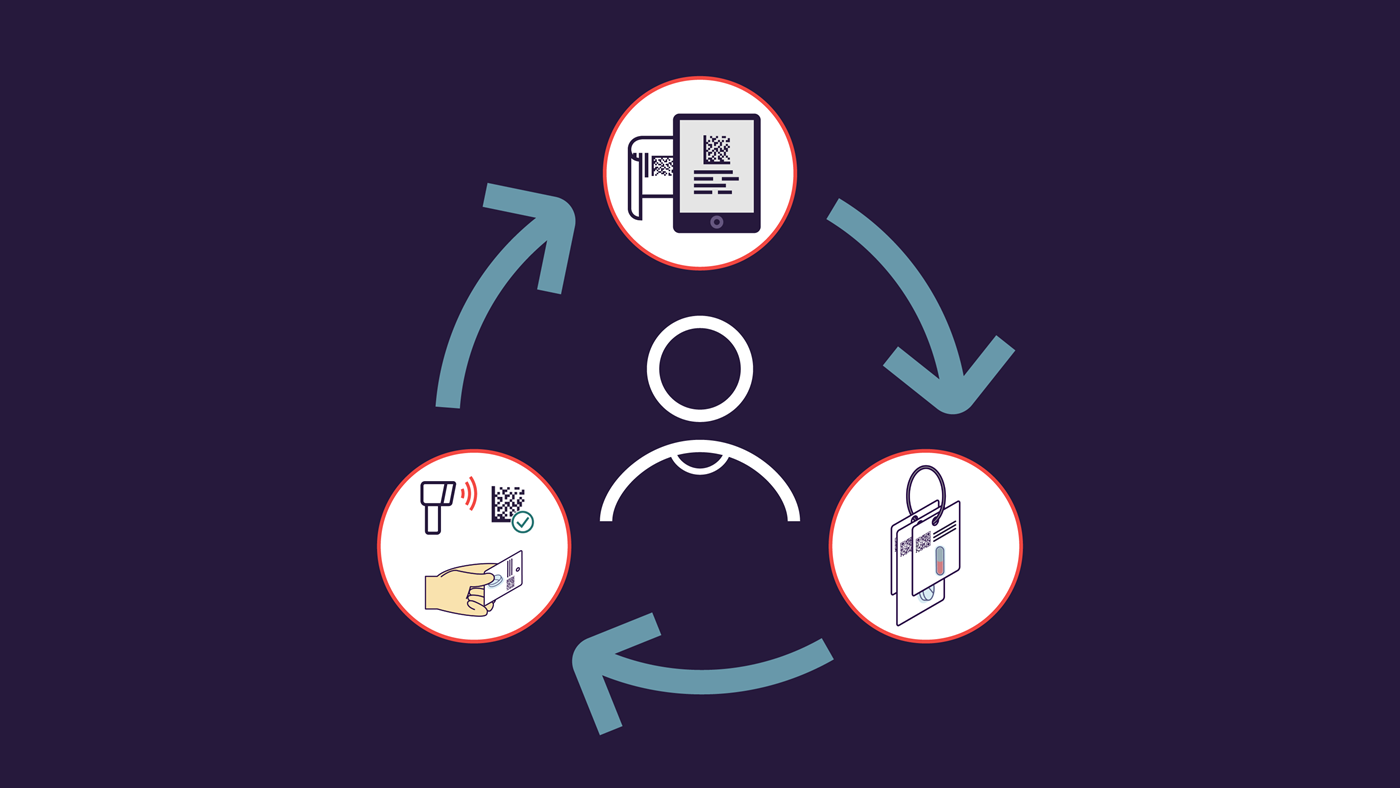
In CLMM, medication administration is seen as a holistic, closed-loop process. The cycle begins with medications that are electronically prescribed by the primary care doctor. The information is transmitted directly to the hospital pharmacy and its associated storage system before it finally reaches the patient’s bedside. Documenting the medication is also part of the process.
An interdisciplinary, cross-departmental team is involved; it consists of doctors and pharmacists, as well as the nursing staff. The linchpin of the process is an electronic prescription system that links medical staff, wards and the hospital pharmacy. It creates the closed loop between all participants, which provides the name for the management system.
How does closed loop medication management work?
Electronic prescription
The patient's file is electronically available and linked to the prescription system. During the prescription process, the medical staff has direct access to all patient-relevant data.
From creation and procurement to distribution – prescriptions are transparently documented. The electronic medical record enables the complete documentation of the patient's hospital stay from anamnesis to discharge.
Validation of prescription and unit dose supply
After prescription, the pharmacist checks and evaluates the medication. The pharmaceutical staff has direct access to the digital medical record in order to check the treatment prescriptions for correctness.
If necessary, patient-specific optimizations to the medication can be made in this step. Both patient and hospital benefit from the pharmacist’s expertise that improves the therapy.
The preparation, production and distribution of individual patient-specific unit dose medications takes place in the central pharmacy. The unit dose package is a small overpack that contains single doses. The advantage is that the medications remain in their original packaging, which avoids contamination. All patient-individual unit doses are then bundled on a ring and distributed to the wards via a hospital's internal pneumatic tube system.
On the wards, the nursing staff administers the dosed medication to the patients. Each unit dose ring carries a specific label that shows the patient's name and important dosage and intake information. The administration is noted in the electronic medical record and therefore traceable.
The advantage is that the patient-specific label is not located on the individually packaged medication itself, but on a separate carrier. Patient-related data can thus be easily removed, so that the medication can be returned to the storage system in case it wasn’t needed due to early discharge or a change in therapy. This reduces medication waste.
Why were unit doses introduced in the hospital?
Unit doses are what makes medication management in the form of a closed-loop process possible in the first place. Thus, both unit doses and the CLMM lay the foundation for preventing errors in the administration of medications.
Unit doses ensure that people in inpatient care receive their individually required medications and take them as prescribed.
What do pharmacies do as part of unit dose care?
The additional control that is possible thanks to the transparent documentation of all individual steps of the therapy enables pharmaceutical professionals to optimize the treatment. Errors in the prescription are detected more quickly by applying the two-man rule. This not only ensures the correct treatment of patients, but also avoids lengthy and costly legal negotiations. Bureaucratic expenses resulting from a lack of drug safety are also prevented.
How does the introduction of the closed loop become a successful project?
Digitalization of all processes
The first step towards CLMM is the digitalization of all medical records, patient files and internal processes in the hospital. The hospital pharmacy needs a reliable IT infrastructure that enables digital inventory. Besides that, hospital staff must be trained to use the electronic systems.
Automation
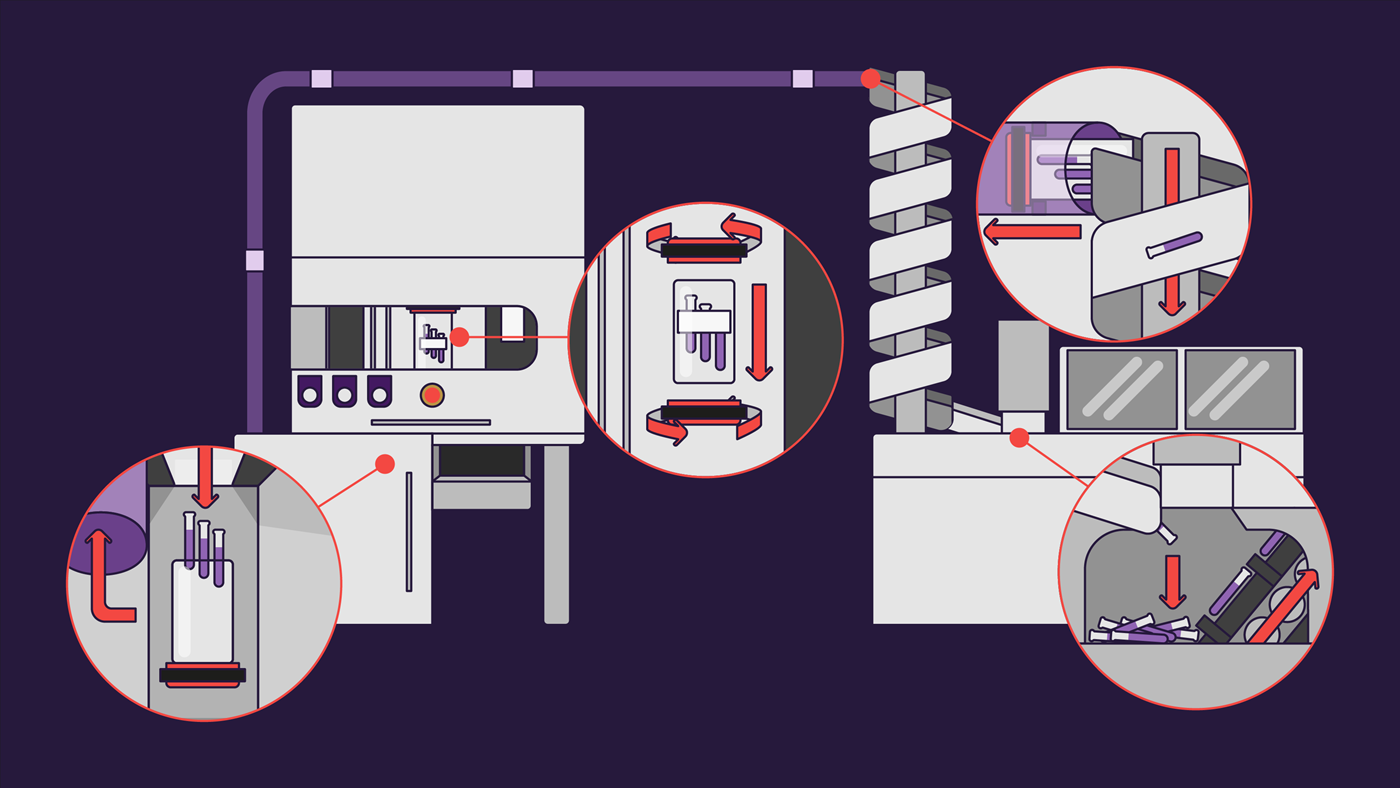
During the automation of the processes, all individual steps of the system are linked with each other. It requires machine support to efficiently and quickly implement the electronically incoming data requests. A modular packaging and dosing system such as the automated unit dose system PillPick can dispense drugs in patient-specific therapies and distribute them to the different parts in the hospital by the use of an internal transport system.
Advantages of closed loop medication management
Patient safety increases as soon as the probability of errors is reduced by the CLMM. This ensures drug therapy safety. The medication process is completely transparent and standardized in the electronic system.
A brief overview of the advantages of the CLMM:
- Relief of personnel through standardized and electronic processes
- Quality assurance through pharmaceutical control of all prescriptions
- Automation reduces manual errors in medication delivery
- Unit dose supply reduces errors in preparation and administration
- More efficient workflows across departments
- Saves time for nursing staff
- Cost savings
Conclusion: closed loop medication management ensures greater patient safety
Even if the transition to CLMM requires a certain amount of time and financial effort on the part of the hospital, it is worth it in the long run. Patient safety increases considerably and the unit dose reduces treatment and administration errors, which saves patients' lives, costs and makes it possible to deploy staff more efficiently. CLMM also promotes quality assurance and efficiency through full transparency.
About the author Guest author